63 yr OLD DIABETIC SINCE 10 YRS SOB, PEDAL EDEMA SINCE 2 MONTHS
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
UNIT 2 ADMISSION
Dr.VAMSHI KRISHNA (INTERN)
Dr.PRADEEP (INTERN)
Dr.JAYANTH (INTERN)
Dr.ISMAIL (INTERN)
Dr.YAMINI (INTERN)
Dr.AMULYA (INTERN)
Dr.PRADEEP (PG 1st YEAR)
Dr. NIKITHA (PG 2nd YEAR)
Dr.SUFIYA (PG 3rd YEAR)
Dr. SATHISH (PG 3rd YEAR)
FACULTY: Dr. VIJAYALAKSHMI
Case presentation:
63year old male with history of diabetes since 10years now on human mixtard
one year ago when he went for regular check up he was told to have high creatinine but he did not have any symptoms at that time
3months ago he developed pedal edema gradually progressed upto knees and since 2months he had sob, decreased urine output for which he was started on dialysis.10sessions of dialysis done till now.
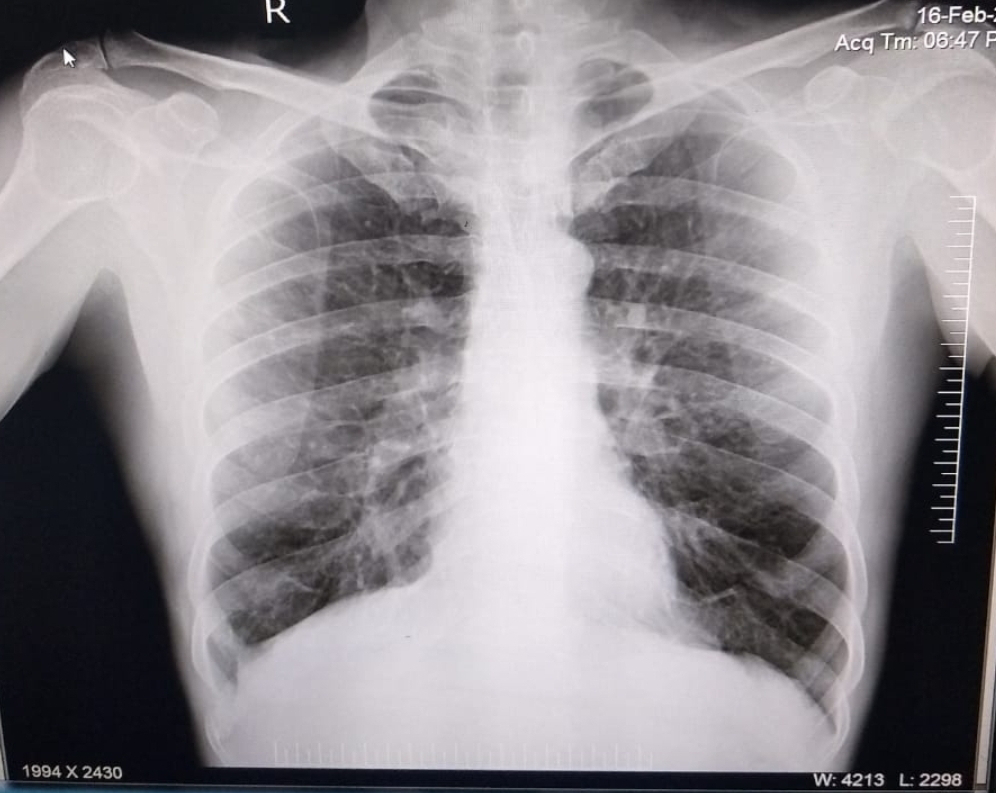
Patient complained of SOB immediately shifted to ICU and found falling saturation (SpO2 <60%).
Pre intubation vitals
Patient drowsy, sweating.
Bp : 180/90 mmHg,PR : 188bpm,
RS - B/L crepts +,diffuse,CVS-S1,S2 +,P/A-distended
Inj.Lasix 120 mg was given to decrease the over load and pulmonary edema .Then patient suddenly went into cardiac arrest 3 cycles of CPR done ,
Inj.Adrenaline 2cc IV/stat given ,
patient revived pulse palpable and BP recordable.
lnj.midaz 2cc IV/ stat was given.
Patient was Intubated with ET-7.5
Post intubation vitals :
BP- 160/90 mmHg,PR - 183 bpm,
CVS - S1,S2 +,B/L crepts +
As HR was high i.e., 200bpm ,
Inj.Adenosine 18 mg IV stat in total was given.
Patient stabilised and connected to ventilator ACMV(VC) with
P support:12,FiO2- 100,PEEP-5,VT -420ml,SpO2 -100%.
RR - 46cpm
Inj.Midaz 2cc IV and Inj.Atracurium 2 amp (5ml) in 45ml NS @15ml/hr.
As patiet was not tolerating patient ventilator mode was changed to CPAP(VC).
RR-25cpm
then Inj.Atracurium 20ml/hr
Patient wasn't tolerating other modes and in V/O high plateau pressure and RR total ,more was changed to SIMV -VC mode.
81MV -VC-mode
PEEP-6cm of H2O
VT-420 ml
FiO2-100%
RR-16cpm
O/E: patient drowsy,BP-130/70mmHg,PR-113bpm,
CVS-S1+,S2+
RS-BAE +, Clear
P/A- distended,BS- sluggish
CNS - GCS-E2VTM3,pupils-B/L mid dialated non reactive to light
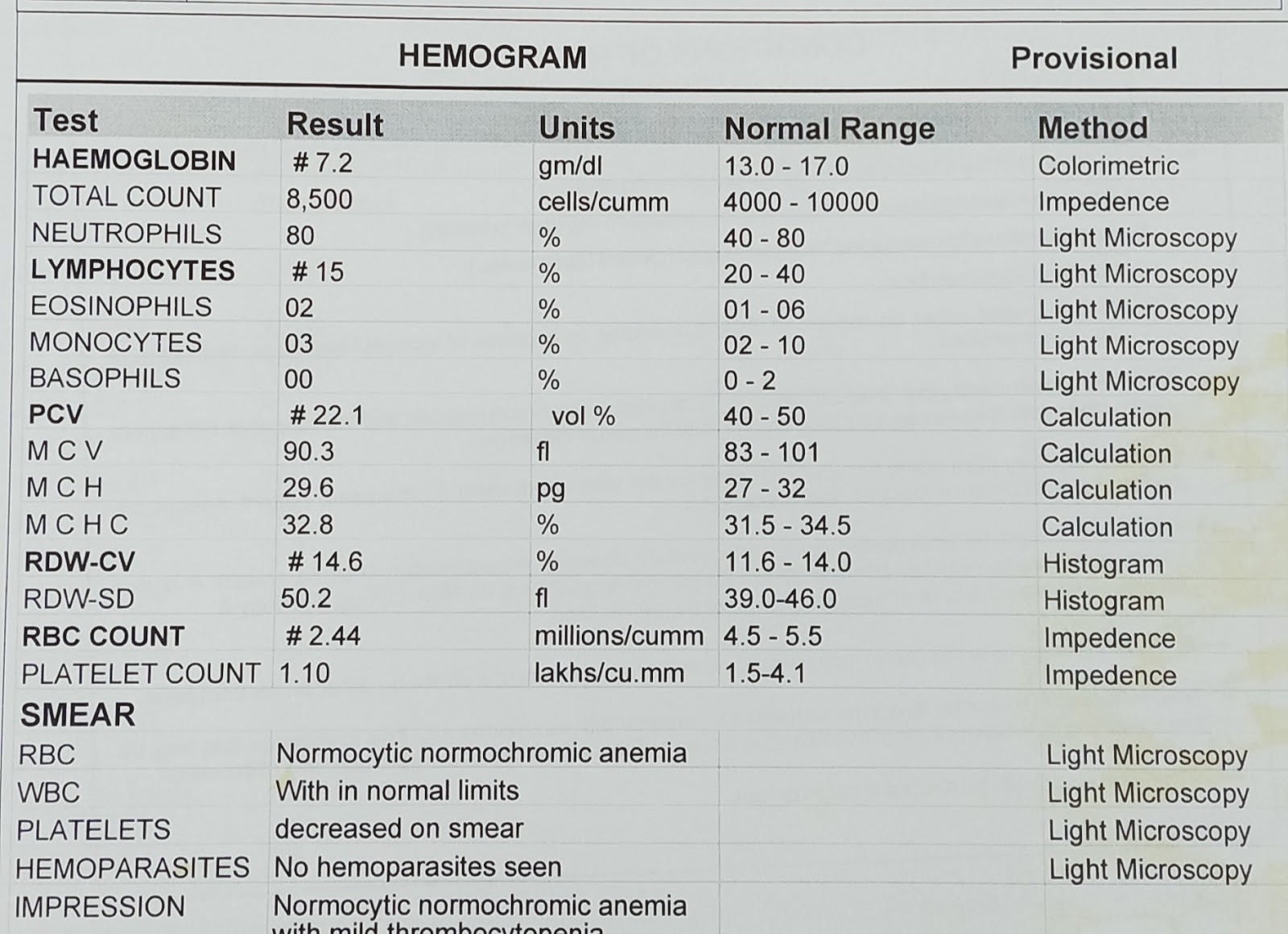
INVESTIGATIONS
DAY 1
HEMOGRAM 19/1/2021
TREATMENT
DAY 1
PER ABDOMEN DISTENDED
INJ. LASIX 120 MG WAS GIVEN TO DECREASE THE OVERLOAD AND PULMONARY EDEMA
pt was suddenly went into cardiac arrest 3 cycles of CPR done, inj. adrenaline 2cc iv/start pt was revived pulse palpable, BP recordable after revived pt was given inj. glycopyrolate (1amp) iv start and inj. midazolam 2cc iv start as heart rate was high inj. adenosine 6 mg iv start as rate was not decreasing again inj. adenosine 12 mg followedby 10 ml ns was given pt stabilised and connected to ventilator
DAY 2
propped up posture
air/water bed
inj. pan 40 mg/iv/od
inj.zofer 4mg/iv/tid
inj.monocef1g/iv/bd
inj.lasix 40 mg /iv/tid
inj.dexmiditomidine/iv/6ml/hr
inj.atracurium@20ml/hr iv
T.ecosporin- av75/20mg/rt
T.ivabradin 5mg/rt
RT FEEDS MILK+protein powder
BP/PR/SPO2 CHARTING HOURLY
DAY 3
propped up posture
air/water bed
inj. pan 40 mg/iv/od
inj.zofer 4mg/iv/tid
inj.monocef1g/iv/bd
inj.lasix 40 mg /iv/tid
inj.dexmiditomidine/iv/6ml/hr
inj.atracurium@20ml/hr iv
T.ecosporin- av75/20mg/rt
T.ivabradin 5mg/rt
RT FEEDS MILK+protein powder
BP/PR/SPO2 CHARTING HOURLY